Nursing staff are much less enthusiastic about the conditions in hospitals than the patients who are treated in them, concludes the PhD research by AnneMarie Eijkelenboom. This is often due to a mismatch between a building’s design and its users.
Much research has been carried out on the well-being of hospital patients, yet we know little about that of hospital staff. Eijkelenboom thought it was high time for a change. In an extensive survey, she quizzed 556 hospital employees about their working conditions. Many respondents proved to be dissatisfied with the temperature and daylight in the outpatients’ area where they worked, and found the air too dry. No less than half of the respondents suffer from dry eyes, and more than a third are affected by headaches. A third of those surveyed also report a low level of social comfort; hospital staff experience too many distractions and too little privacy. “Hospitalworkers are more dissatisfied than workers in office buildings,” says Eijkelenboom, who is an architect at EGM architects. “This really needs to improve.”
Indoor environment
Eijkelenboom visited six hospitals and saw 127 rooms in order to identify correlations between complaints and building characteristics. She found that the complaints are often related to a building’s design. The lack of a window onto the facade or corridor can contribute to headaches, and it is very important to have sufficient daylight. Dry eye problems are also related to building characteristics that affect indoor air, such as the use of a thermal wheel or failing to clean ventilation grilles frequently enough. According to the research, cleaning less than once a month is a bad idea, as it has been known for some time that a poor indoor environment also negatively affects absentee rates.
Office spaces score poorly
Taking a closer look at the survey data revealed a strong correlation between satisfaction with temperature, sound and light and the type of room in which someone works. Satisfaction with the comfort level was highest for the consultation and examination rooms, whereas it was lowest for the office spaces. “The explanation could be that more attention is paid to the design and furnishing of consultation rooms, because patients go there”, thinks Eijkelenboom. Office spaces score poorly due to the lack of privacy and too many distractions. During the COVID-19 pandemic, staff also had concerns about ventilation and inadequate contact with patients.
Strike a balance
There are no simple rules for improving the situation, according to the research. Hospitals do their best to provide good air conditioning in what are often complex and large buildings, but this has not stemmed the complaints about dry air. “It’s tricky for hospitals to strike a balance between comfort and sustainability.”
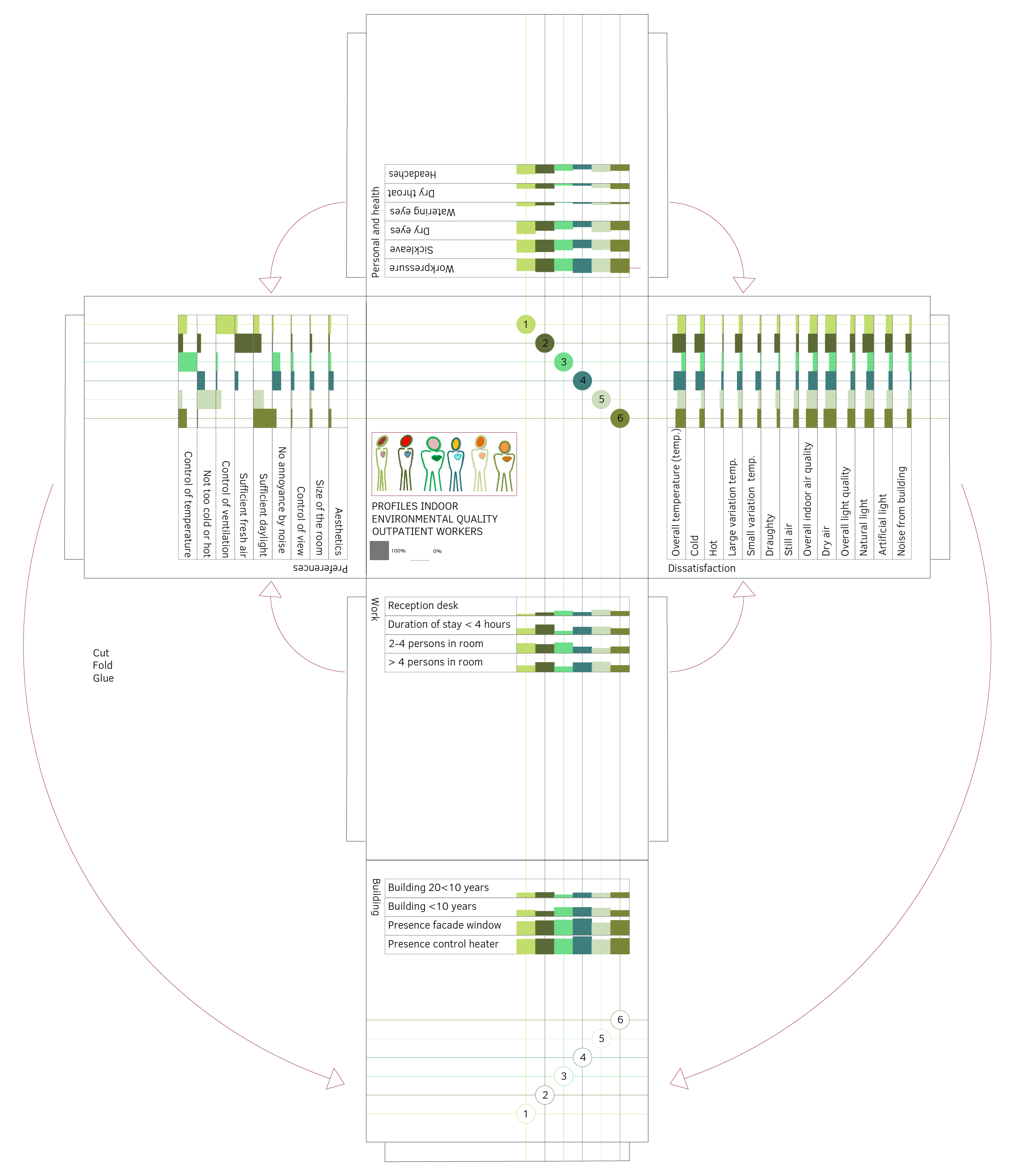
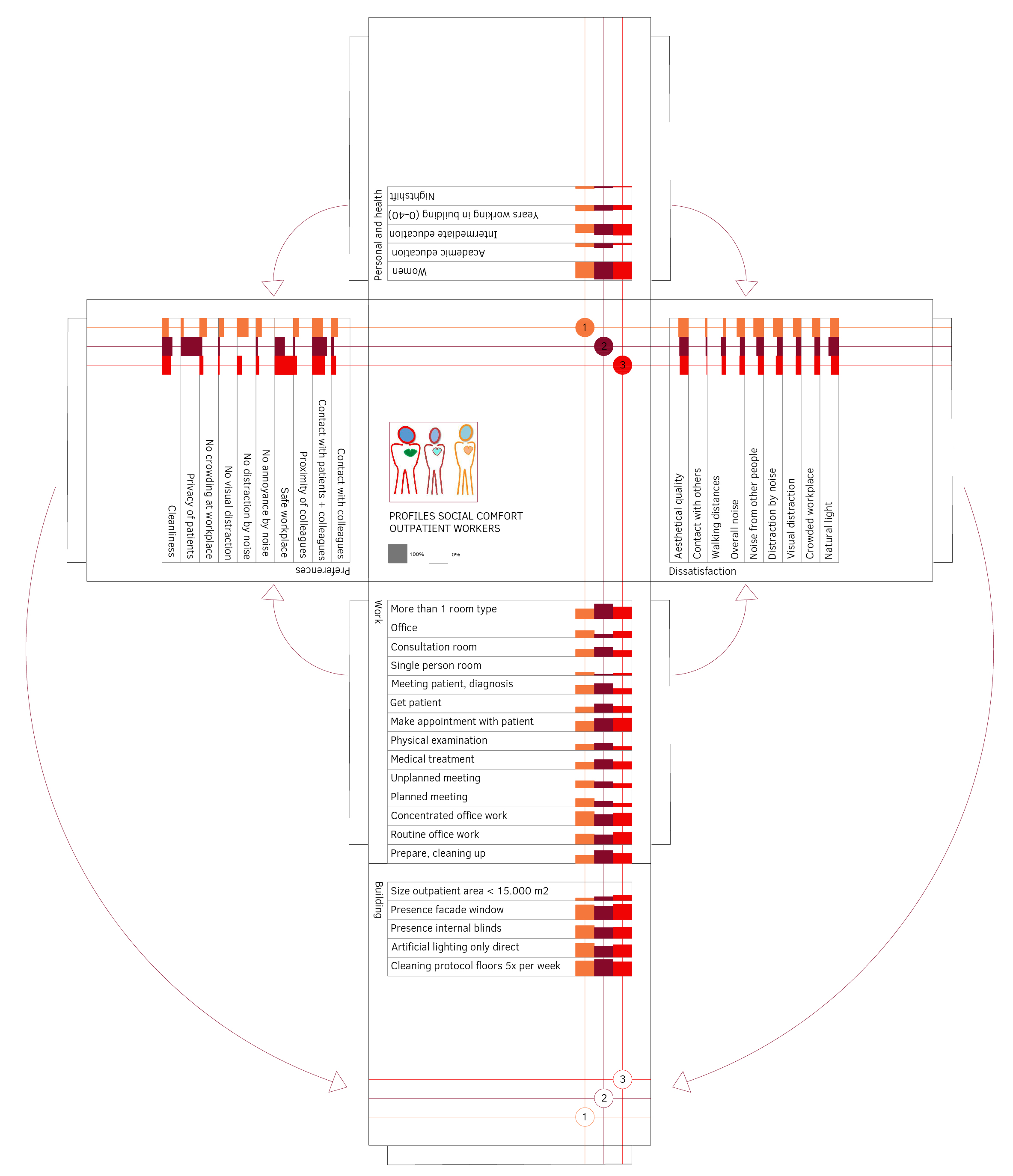
What’s more, every employee has their own idea of what is comfortable. In order to do justice to this, profiles have been created that provide more insight into the relationship between preferences for comfort, work and health. This shows, for example, that those with many complaints consider ventilation to be very important, whereas those who spend a long time working in the same room think that daylight is important.
When people have control over their own environment and a building offers flexibility, also at the micro level, you can do most justice to everyone’s personal preferences. “If staff are able to open a window or door, adjust the thermostat a few degrees or move to a different – more pleasant – room, this adds to their experience of comfort,” says Eijkelenboom. “People adapt to their environment, but it is better if they are also able to adapt the rooms they are in.”
Published: October 2021
More information
- PhD thesis 'Understanding comfort and health of outpatient workers in hospitals, a mixed-methods study'
The doctoral research was made possible by co-financing from Daikin Netherlands and the provision of time by EGM architecten.