In Delft and Rotterdam, Wouter Serdijn and Christos Strydis are collaborating on a network of sensors and stimulators for the body. By picking up signals and sending the brain a rapid wake-up call, they hope to be able to predict and prevent epileptic fits. ‘If we can close the loop, we’ll have the technology ready within three years.’
Epilepsy is a collective name for disorders of the brain caused by a change in the brain cells’ electrical activity. These neurons suddenly become overactive, firing their electric signals uncontrollably. This sometimes results in a ‘short-circuit’: seizures where a patient loses consciousness or has involuntary muscular spasms. For the more than 200,000 Dutch people with epilepsy, this can be very dangerous. But what exactly happens during an epileptic fit? What exactly do the overactive brain cells do? And how can we influence that process? Wouter Serdijn, Professor of Bioelectronics at TU Delft, is trying to answer these questions by researching and designing technology for monitoring, diagnosing and treating epilepsy.
In a fit, all the neurons start jumping at the same time. In major seizures especially, they literally become exhausted.
Get-together
‘Do you know the band Rage against the Machine?’ asks Wouter. ‘I always compare epilepsy to their song Killing in the name of. Epilepsy experts say I’m mad for making the comparison, but that’s what the signals remind me of. In the chorus, everyone’s jumping all over the place.’ That’s what happens with brain activity during a seizure. It amplifies the signal, reducing the exchange of information to zero. The result is an epileptic fit.
That kind of seizure can really affect patients’ quality of life, says Wouter. ‘All of those 200,000 Dutch people are prohibited from driving or using heavy machinery.’ They also need to exercise constant caution in their day-to-day lives: stress or flashes of light can trigger a seizure. In addition, drugs are not always successful in preventing seizures. ‘In major seizures, the brain cells simply break down. They literally become exhausted and die.’ Wouter is therefore applying a technological perspective in his search for solutions that could help the body prevent these “wayward get-togethers” between brain cells.
Wake-upcall
As Professor of Bioelectronics, Wouter is working on technology that interacts with the electricity in the body, attempting to measure and influence it. But, for epilepsy, that’s easier said than done: just like with the crowd jumping up and down, you have little control over it. The entire cerebral cortex – the area of the brain that receives, interprets and analyses information – is involved in the process, says Wouter. ‘So, what you need is a wake-up call for the whole cerebral cortex that can restore normal communication without bringing it to a standstill.’
Together with the Erasmus MC in Rotterdam, he is conducting research into the role of the cerebellum in conveying information. ‘The cerebellum regulates the body’s motor movements and it branches into all parts of the brain. These connections can help us to close the loop: accurately detecting where and when a seizure develops, making an intervention that can reach all parts of the brain and then measuring the effect of that intervention.’
Rocket science with patients
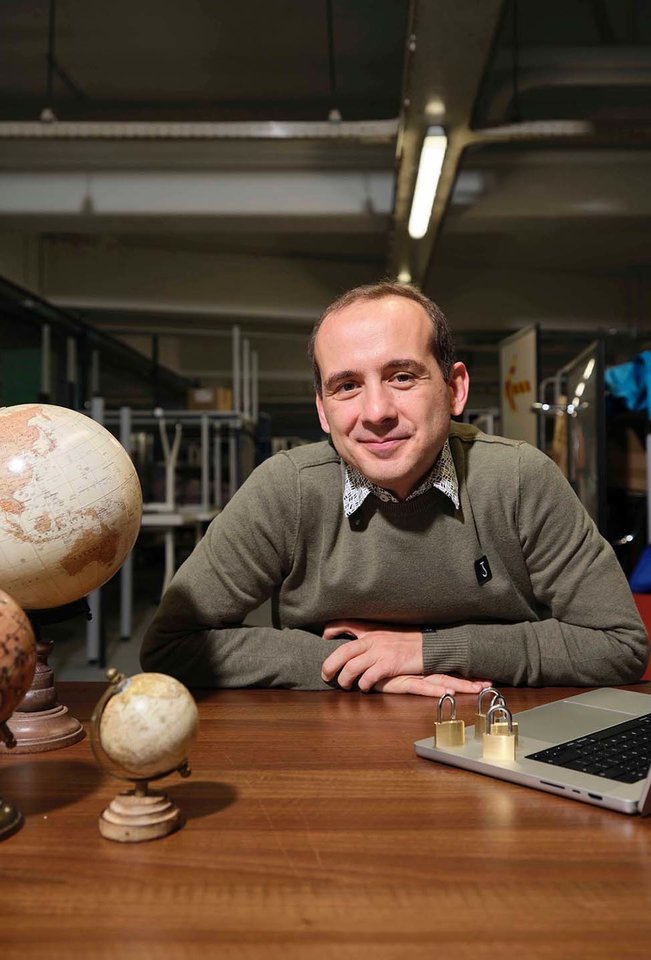
Christos Strydis is one of the researchers of Erasmus MC who is bridging the gap between the clinic and the technology. A computer engineer with roots in Delft, he works as an assistant professor in the Neurosciences department. ‘I sometimes feel like a translator,’ says Christos. ‘In Rotterdam, there’s a lot of knowledge about brain function and how the different parts of the brain interconnect and the people in Delft have a lot of experience in building technological solutions.’ Christos has to speak both languages. ‘Some of the bioelectronic solutions we devise for neurosciences are not rocket science, but others are. If we stayed in Delft, we engineers would never be able to gain experience with patients.’
If we engineers all stayed in Delft, we would never have experience with patients.
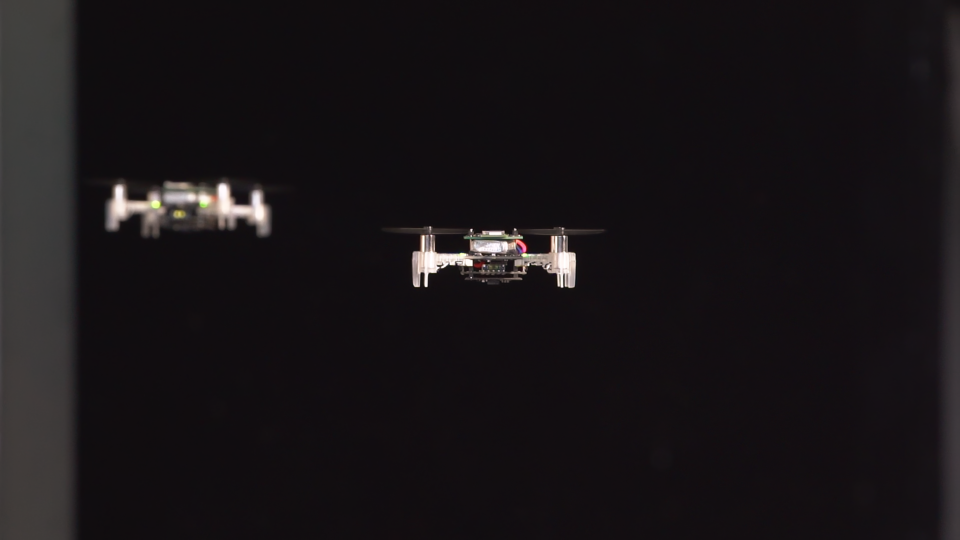
With that in mind, Wouter and Christos are setting up a platform to explore the medical issues surrounding epilepsy from an engineering perspective. They have received a grant from the Delft Health Initiative for their work. Their project ECLEPSys – Ensemble, Closed-Loop, Epilepsy-Prevention System – consists of a prototype for a sensor network made up of implantable and wearable sensors and stimulators. The first group measures signals from the brain and the second links a signal back into the body. The idea is that the signal should stimulate the brain cells in such a way that they revert back to normal.
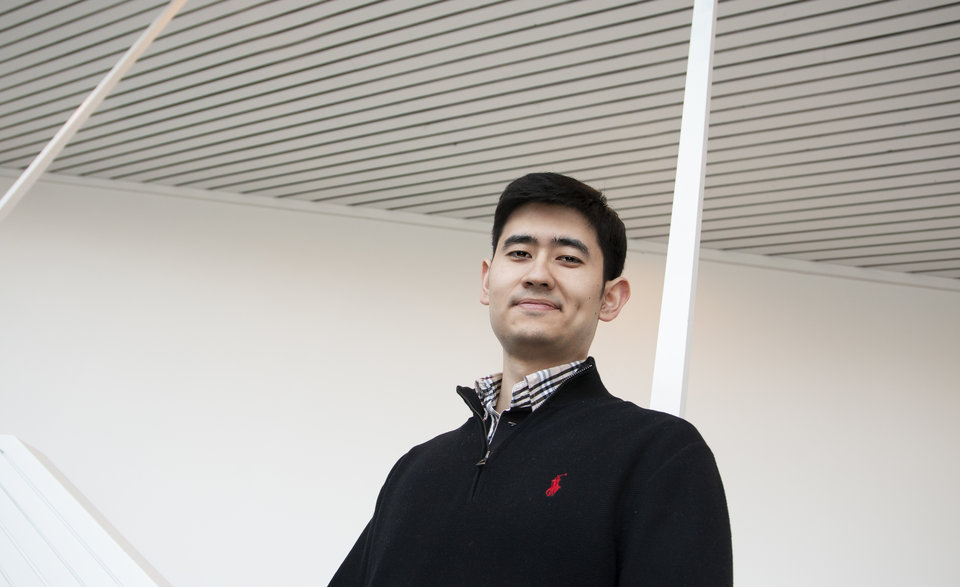
‘It’s actually totally logical for neuroscientists and engineers to join forces,’ says Wouter Serdijn. He is Professor of Bioelectronics in TU Delft’s Faculty of Electrical Engineering, Mathematics and Computer Science. He has spent his academic career in Delft: from his Master’s degree to his appointment as professor. ‘I’m a Delft boy. In some ways that’s actually quite boring. But I just think it’s an amazing place.’ Wouter is one of the few engineers with an innate interest in medical technology. He applies his expertise in bioelectronics to his work on such areas as pacemakers, hearing implants and neurostimulators.
‘You call it boring, but you have quite a few miles on the clock,’ says Christos Strydis. He did his Master’s degree in Computer Engineering in TU Delft where he also completed a doctorate. His career in neurosciences took off in Rotterdam, first as a PostDoc and now a tenured assistant professor with the Neuroscience Department of the Erasmus MC. As an engineer there, he forms a bridge between neurosciences and technology. Together with Wouter, Christos was recently awarded a grant by the Delft Health Initiative to develop the ECLEPSys project as part of Convergence, the joint programme of TU Delft and Erasmus MC in Rotterdam.
Sandbox
ECLEPSys involves building a complete medical body area network (MBAN). This is a partly wireless network made up of nodes, each with its own task: sensors, stimulators and a computer that coordinates the signals with each other. A MBAN is more effective than existing technology because it is measured, adjusted and calculated on or next to the body. ECLEPSys can therefore make a difference in epilepsy in particular, but Christos has even bigger ideas. ‘A MBAN could also be used to treat other disorders: heart arrhythmia, Parkinson’s, migraine or tinnitus. We aim to demonstrate that it is possible to help patients by applying machine learning and algorithms to biosignals.’ ECLEPSys can be compared to a sandbox, where ideas can be tested. ‘Examples could include new sensors, new forms of stimulation and ways of analysing data. But the project also encompasses data security.’
For epilepsy patients, it is hoped that ECLEPSys will bring about a new treatment method, combined with drugs. ‘I expect that this will enable us to suppress or control epilepsy,’ says Wouter. ‘The great thing about this type of neurostimulation is that you just switch it on and it works immediately. And vice-versa: you stop if you no longer want it. That makes treatment personal and targeted. Drugs can never be so fast: they don’t know where in the body they’re supposed to go.’
Work to be done
But that is still some way off, says Wouter. ‘We already have a system that can detect and suppress epileptic fits but it only works with mice at the moment. Their cerebellum is very similar to that of humans.’ By measuring brainwaves and stimulating the cerebellum, Wouter and Christos were able to suppress an epileptic fit elsewhere in the brain. That demonstrates that the principle works, says Wouter. ‘We were able to detect that a fit was coming within 0.4 seconds and stop it.’
But before epileptic patients can start driving again, there’s still a lot of work to be done. The energy management of the sensors and stimulators requires improvement, for example. The technique that Wouter and Christos are using has still not been cleared for use on humans. ‘Our system is still not a network. We’re working on other ways of getting signals into the brain. Instead of EEGs, we’re working on different types of feedback. We know that the body sends signals before a fit starts: sweating, dilated pupils or an increased heartbeat. We need to learn to use that information.’
There is significant variability between patients. That calls for a different approach.
Translating
Before Wouter and Christos can use the system on patients, they aim to make it as efficient as possible first. The collaboration between Rotterdam and Delft is essential in this: the realism of the medical experts in Rotterdam keeps the Delft engineers and their get-things-done mentality in check. ‘We would never have made such progress without our contact with Erasmus,’ says Wouter. ‘Engineers believe in the power of repetition. If we make something twice the same way, it also needs to work the same way. That principle does not work on patients. There is significant variability between patients, and even in the same patient at different times. That calls for a different approach.’
Besides that, it’s not only about the technology, adds Christos. ‘Before rolling this out to more people, you have to discuss such issues as ethics and quality-of-life. You cannot measure brain activity everywhere in the body. Do you really want to burden a patient with all kinds of sensors on his head?’ Despite this, Wouter thinks that the technology behind ECLEPSys can be translated for human use within the foreseeable future. ‘You cannot apply substandard work on people. But I’m still optimistic. If you can predict epileptic fits with the right signals, we can close the loop. Then we’ll have the technology up-and-running within three years.’
Text: Koen Scheerders | Portrait photo: Mark Prins
More stories
Health & Care
Bio-engineering