More people die from treatable surgical conditions than from HIV, malaria and tuberculosis put together. This is what Roos Oosting wants to change with her ground-breaking PhD research into surgical equipment for developing countries. Her goal: to make safe surgery possible anywhere in the world.
When Roos Oosting travelled to Kenia four years ago, many people thought she was ‘also a surgeon’, or that she was perhaps selling surgical equipment. That the Delft Global PhD-fellow within the department of Biomechanical Engineering wanted to know how surgical equipment is used in the African hospitals was a new question. As a part of the programme ‘surgery for all’ of TU Delft professor Jenny Dankelman, Oosting investigated the requirements surgical equipment in Africa must meet. Something which received little attention until recently.
Surgery in Kenya
Oosting contacted a great number of surgeons, biomedical technicians and NGO’s in Kenya, where she lived for several months, and later also in Mozambique and Rwanda. From surveys and interviews it became clear how different the reality is in an African hospital in comparison to one in Europe or North America. Often the electricity supply is unstable, there is a limited access to water -problematic for the cleaning process of equipment- and the maintenance and replacement of parts is much more difficult.
Still, it is common practice to donate medical equipment from hospitals in the West, which is not always successful. The equipment is too complicated to repair or is used differently than intended. “We see that things designed for one time use are in fact reused. They are cleaned with a chemical disinfectant, while the materials are not meant for this. Not all pathogens are washed off this way, which creates a risk of infection.”
Reality in the operating room
If possible Oosting would spend a day with a surgeon. “In the Netherlands we picture an operating room quite differently from what the reality is on the other side of the world. It is incomparable. I would see equipment constantly being dragged from one OR to the next, because there was not enough.”
The most surprising for Oosting was the lack of essential surgical equipment, at places where successful surgeries were performed. “Three out of ten hospitals did not have a heart rate monitor. Some did not have a device to deliver oxygen, or to sterilize the instruments. I remember thinking: ‘I hope I never have to lay on this operating table.’ For me that shows the urgency of my research. Everyone deserves a well organised operating room.”
Designing for Africa
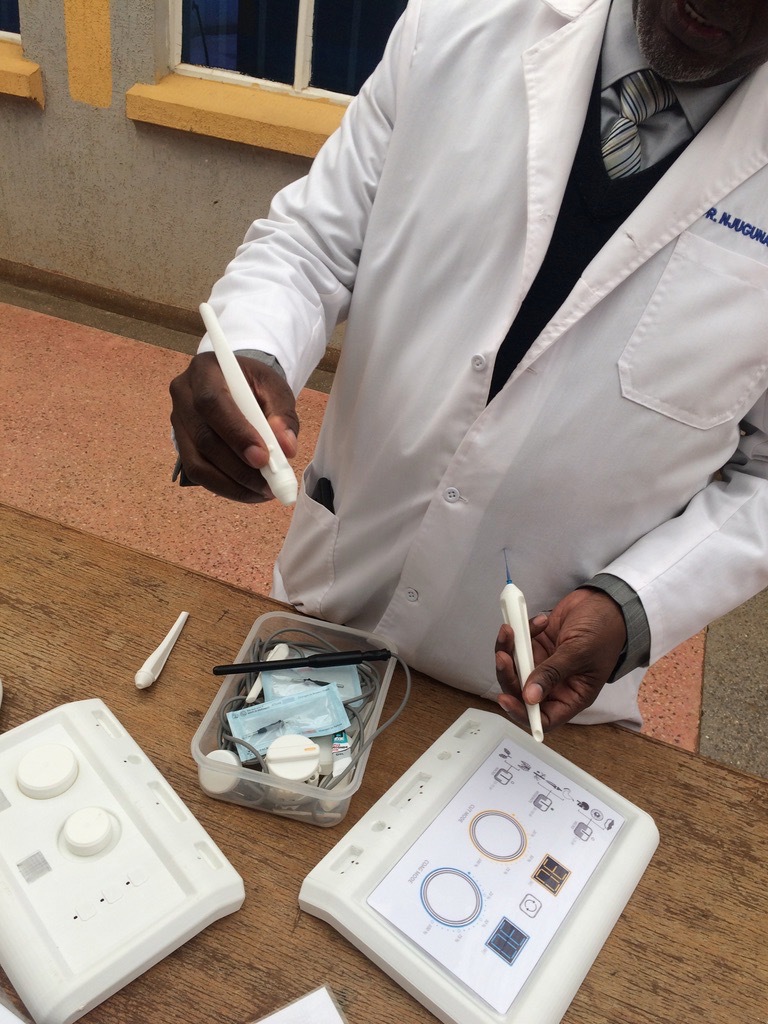
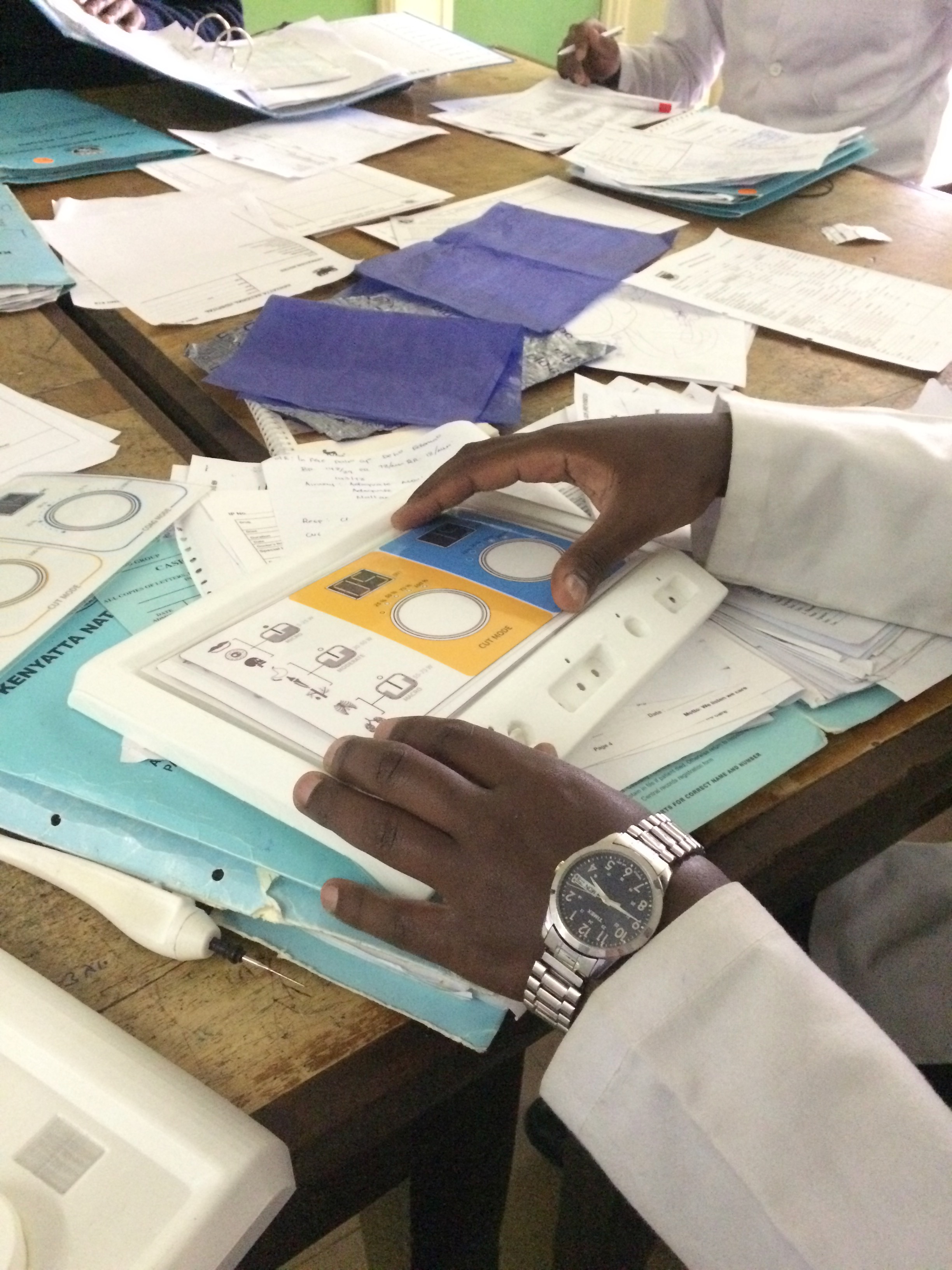
In constant deliberation with local doctors and medical-technical staff, Oosting developed a context-driven design approach for an electrosurgical unit, an important tool used to make incisions and cauterise wounds. “This device needs to be easy to move, thus small and compact, and it has to run on a battery. The accessories have to be reusable and robust. If a bed runs over it, it still has to work,” says Oosting.
Other advices are to make surgical equipment meant for Africa suitable for chemical cleaning, and to keep the interface and technical wiring simple. Meaning minimal knowledge is required for its use and it will be easier to repair. “Maintenance is hard to organize, so you can count on it that people will open it up themselves and try to make it work again. So it is better to facilitate that.”
Local cooperation and international network
Oosting is perhaps most proud of the extensive network she built between TU Delft and the biomedical technology sector in Kenya, Mozambique and Rwanda. In addition to the intensive contact with local surgeons and hospitals also internship projects were set up in three different locations in Kenya. Providing the new generation of biomedical engineers with insights in the local context and facilitating an exchange of knowledge. For example, together with master students Oosting developed software to keep track of the inventory and maintenance of equipment for a hospital in Eldoret, about an eight hour drive from Nairobi.
“It is special that there now is a network people can continue working with. There are many students who now want to do their internship in Africa, before there was no possibility for this, I think that is a very valuable result.”
Future
The ultimate goal is to facilitate the step towards minimal invasive surgery, or keyhole surgery, in Africa. This operation technique which uses very small incisions minimizes the infection risk tremendously, but it also requires more specialized surgical equipment. “People are already trained to do this, now the equipment just needs to be there.” Oosting trusts this can become a reality in the near future. “I have high expectations of the development of Africa.”
The brand new doctor is not finished by far. Together with a colleague she started the company CASE (www.case.health), to continue building bridges between the development of surgical equipment and the reality in developing countries.

Jenny Dankelman