Safe and affordable red blood cells without donors
The production of cultured red blood cells (cRBCs) holds the promise of being a potentially unlimited source of cells that could meet the increasing demand for red blood cell transfusions. TU Delft and Sanquin have now developed an improved process for the production of these cRBC’s. It also allows for greater control over the quality and safety of the cells compared to the current donor-dependent system. Additionally, cRBCs could be utilised for novel therapies in which cells serve as carriers of therapeutic molecules.
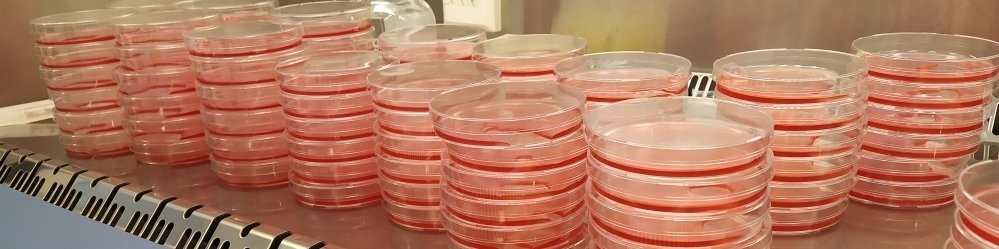
“Until now, cultured red blood cells could only be produced in very small quantities”, says Joan Gallego, who will defend his PhD thesis on this topic on Friday, 10 November in Delft. “These cells originate from precursor cells, called erythroblasts. In the human body, production occurs through a process (erythropoiesis) in our bone marrow. Here, erythroblasts have an ideal growth micro-environment with the exchange and transport of growth factors, as well as the removal of waste products. Prior to entering the bloodstream, the precursor cells differentiate into red blood cells by significantly reducing in cell size, increasing in hemoglobin content, and ultimately expelling their cell nucleus completely, thereby losing the ability to proliferate.”
This fascinating project has also been a very stimulating experience for the many MSc students who graduated during the PhD project. We are not at the end of the developments.
Aljoscha Wahl, promotor, now at Erlangen but involved in most of the research at TU Delft.
Labor-intensive
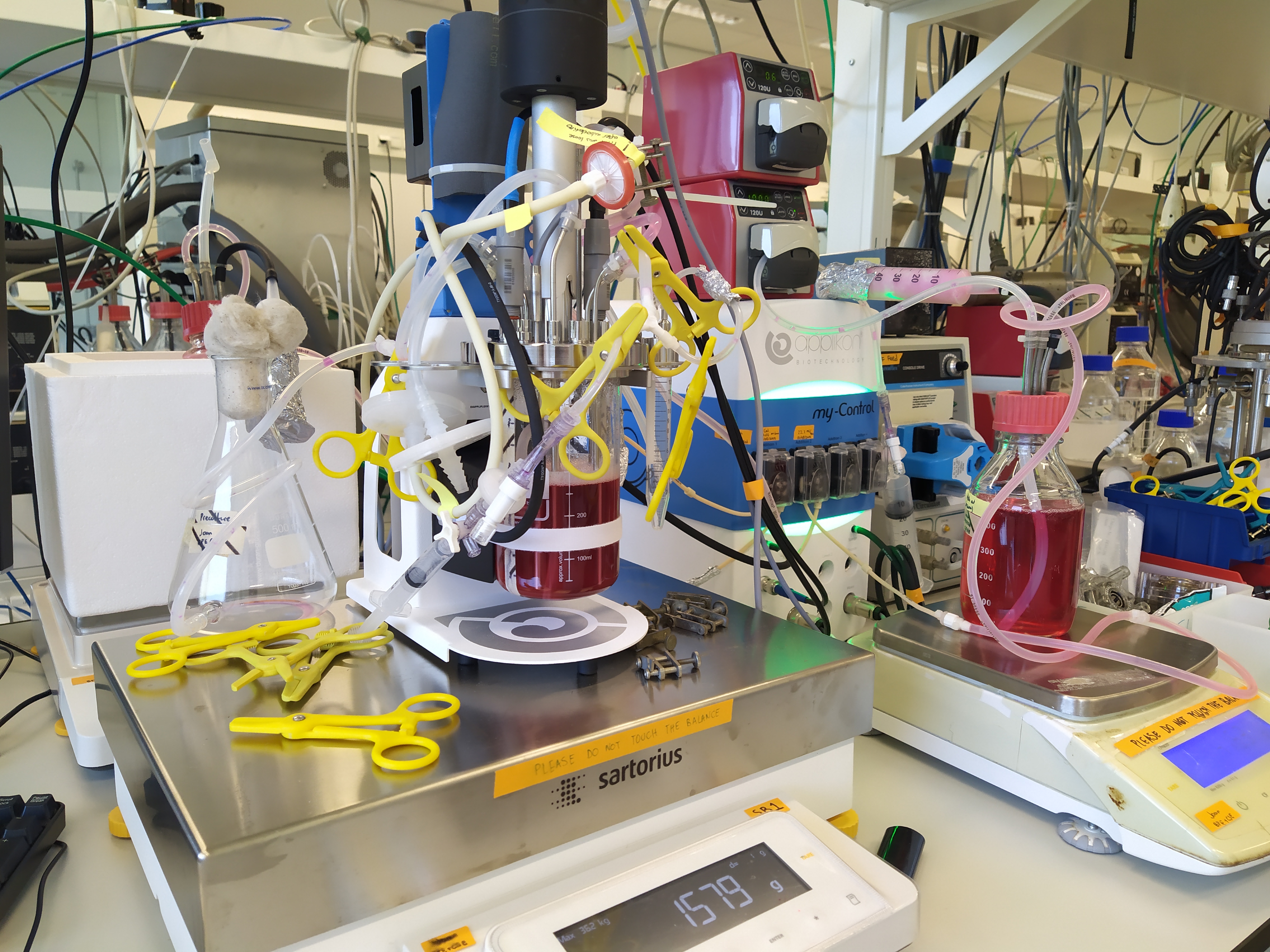
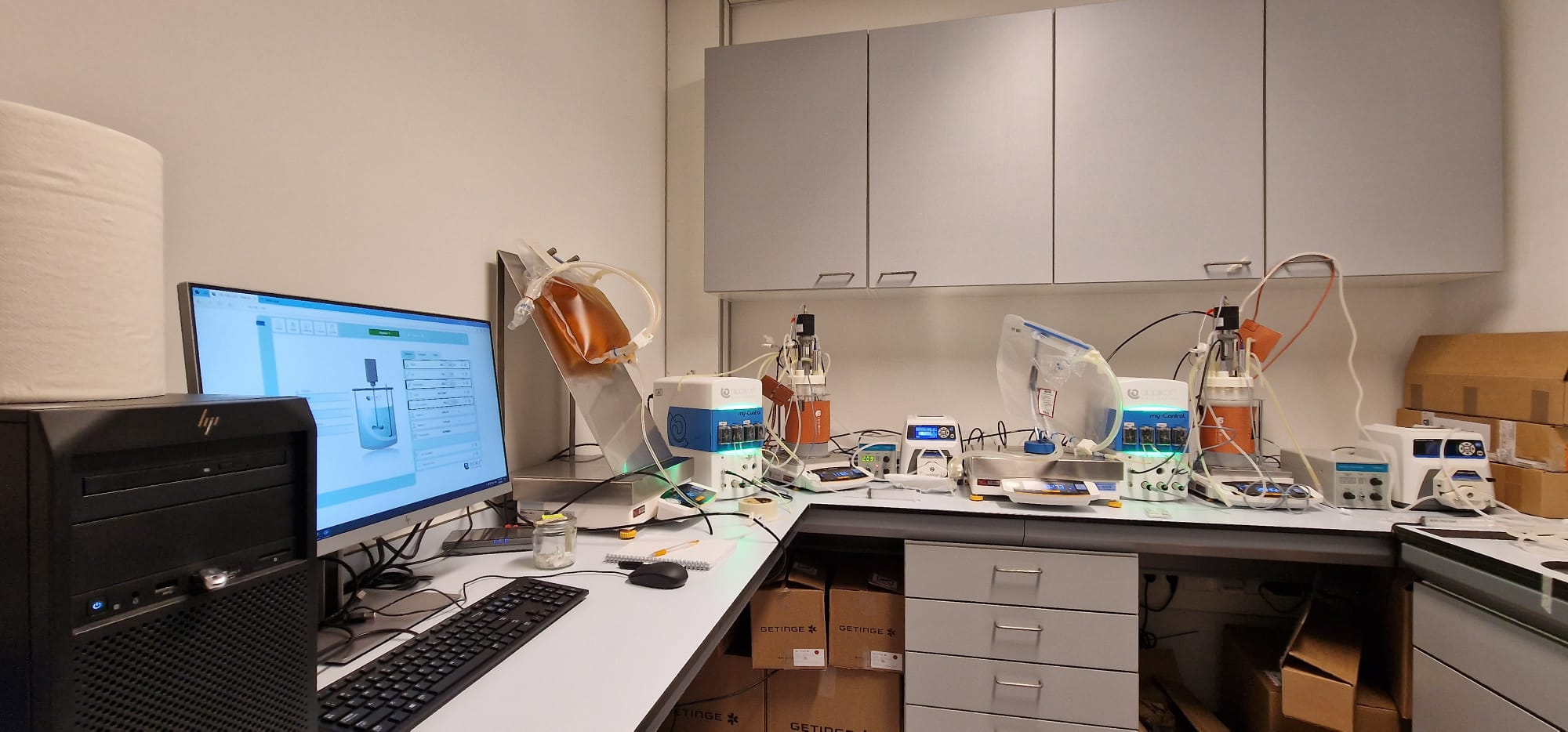
The current technology for the production of cultured red blood cells is very labor-intensive, operates on a rather small scale, and requires large volumes of very expensive growth medium. Gallego developed operating conditions in standard bioreactors for the rapid growth of precursor cells to achieve very high cell concentrations, while ensuring differentiation towards red blood cells only at those high cell concentrations. The 0.5 litre bioreactors that Joan used are considered very small scale according to biotech industry standards, but they are two orders of magnitude larger than the millilitres of current static culture systems. The TU Delft-Sanquin team successfully scaled the process to 3 litre bioreactors, opening the pathway to commercial reactors exceeding 10,000 to 25,000 litre and reducing the capital cost per transfusion unit by 2-3 orders of magnitude.
In our first discussions in 2016, Sanquin expressed satisfaction if RBCs could be provided for patients with specific diseases such as sickle cell disease, only. We at TU Delft challenged Sanquin to aim for mainstream blood transfusion targets. We need to ask big questions to get big answers. I think Joan and the wider Sanquin-TU Delft team have jointly paved the way for this. This is a major step and underlines the strength of the multidisciplinary approach.
Luuk van der Wielen, promotor from the Department of Biotechnology at TU Delft and Bernal Institute at the University of Limerick
Costs
“In addition to increasing volumetric productivity (the number of red blood cells per bioreactor volume and time), we needed to reduce the costs of the expensive growth medium”, Gallego adds. “Growth factors and proteins added to the medium are major contributors to the cost. Holotransferrin, an iron-carrying protein which plays a role in hemoglobin synthesis, is a main cost driver. We were able to successfully replace holotransferrin (with a GMP-compatible iron-loaded chelator) at a fraction of the cost, especially in the differentiation phase. No toxic effects were observed.”
We still have to solve the purification of the RBCs by removing nuclei. But we are optimistic and estimate that costs for a cultured transfusion unit can be reduced by an order of magnitude with the current findings. A bigger challenge is organising the paperwork for regulatory affairs. Therefore, I would be surprised if we can have it ready at transfusion scale and approved for pharmaceutical production before 2030.
Marieke van Lindern, promotor and Head of the Department of Hematopoiesis at Sanquin Research