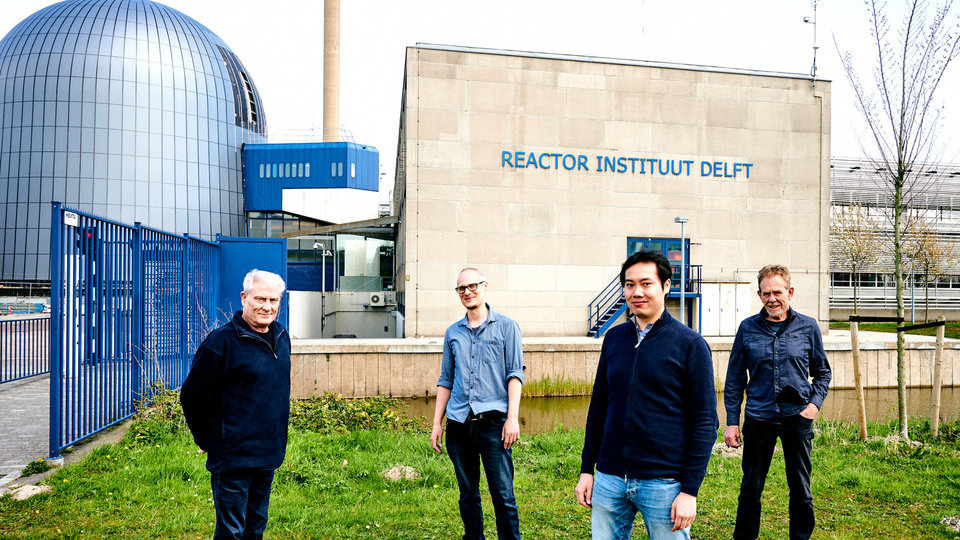
An outpatients’ centre for cancer patients is certainly not the first thing you would expect to encounter on TU Delft campus. ‘But the decision to choose Delft as the location for the Holland Proton Therapy Centre has actually proved to be a very smart move’, says Medical Director Prof. Marco van Vulpen*. The location alongside the TU Delft Reactor Institute offers an excellent opportunity for clinicians and engineers to collaborate closely.
When setting up the Holland Proton Therapy Centre (HollandPTC), the founders envisaged an attractive workplace, where people would have easy access to each other. A place where ideas can emerge that medical experts or engineers might not have come up with if they were not working together so intensively. Ideas like the one to improve medical imaging using new x-ray technology that enhances the visibility of soft tissues during proton therapy, a technique that the engineers are currently developing. Medical experts were unaware that this was possible in theory. The x-ray images that they are currently still using during radiotherapy to monitor the location of a tumour in real time mainly show the bones.
This radiotherapy at HollandPTC involves a beam of protons that advance towards a tumour at enormous speed. A cyclotron and large magnets accelerate the protons to two-thirds of the speed of light. When the proton beam moves through the body, only minimum energy is released, causing very little damage to healthy tissue. Virtually all of the energy is released in one place, where the protons come to a standstill. The depth at which this happens can be adjusted, making it possible to target specific tumour tissue.
‘You might compare it to the point where the ball hits the pins on a bowling alley’, explains Marco van Vulpen. ‘The ball loses almost all of its energy at that point.’ The big advantage of this is that there are fewer side-effects because healthy tissue sustains hardly any damage.

Although many patients are already benefiting from this, the technology is still in a relatively early stage of development. ‘There’s still plenty of room for improvement.’ The suppliers of medical equipment appear to agree. Industrial partners, such as Varian, RaySearch, Siemens and Philips, have contributed more than €10 million for research at HollandPTC. There are currently around forty doctoral candidates working at the centre, which opened its doors to patients four years ago, and funding has been arranged for a further ten young researchers. The doctoral candidates work at HollandPTC and TU Delft, as well as two university medical centres: Erasmus Medical Center and Leiden University Medical Center.
Faster dose prediction
Every year sees doctors referring increasing numbers of patients to proton therapy centres. However, the radiation equipment has only limited capacity. For this reason, research is not only focusing on how the technology can be improved, but also on the issue of which patients can benefit most from proton therapy.
Another important objective is to find out how the limited number of healthcare staff available can treat more patients per day than is currently the case. Developing new methods of calculation that enable medical experts to precisely predict the required dose more rapidly can help with this. The Reactor Institute's expertise in calculation methods for radiation proves useful for this purpose. In addition, research into ‘sensitizers’, chemicals that increase the vulnerability of tumour cells to proton radiation, may also reduce the duration of treatment in the longer term.

Cup of coffee
Close collaboration between doctors and engineers does not always come easily. ‘They basically speak different languages and their work involves totally different timelines’, explains Van Vulpen. Besides this, doctors are always working against the clock in order to start their patients’ treatment as quickly as possible and maximise the chance of survival.
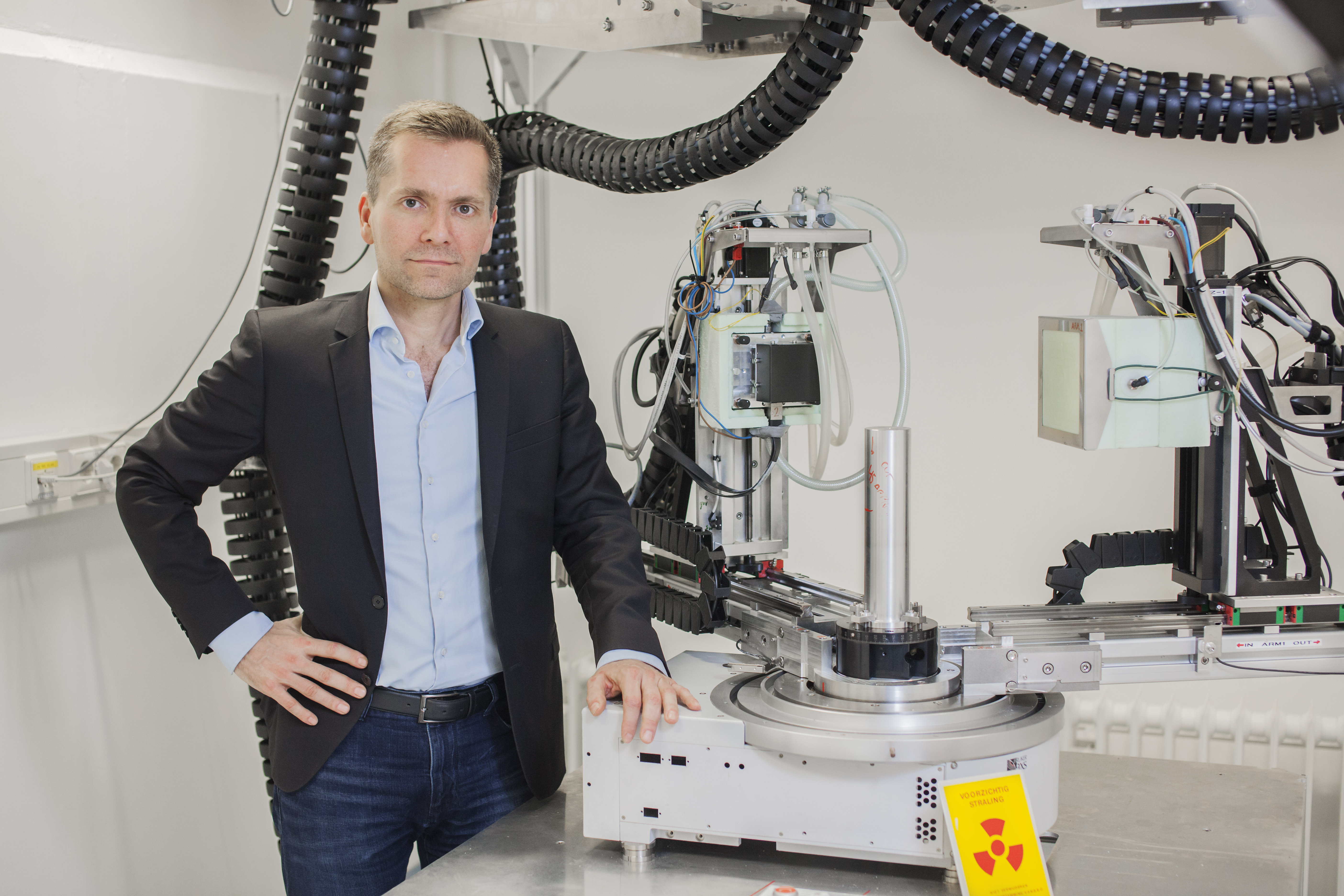
‘As engineers, it’s quite normal for us to work on a new technology for five years or more. That means that doctors have to spend years investing some of their time collaborating with us while continuing to believe that the result will turn out to be a valuable innovation’, explains Dr ir. Dennis Schaart, member of the HollandPTC R&D Programme Council and Head of the Medical Physics & Technology section in TU Delft's Radiation Science & Technology (RST) department.
On the other hand, engineers also gain a wider perspective. ‘We regularly go to drink a cup of coffee with people in the clinic. Since they’re our neighbours, it’s easy to just drop in. We want to find out what questions they have and what the preconditions are for using new technology and then test out and improve ideas through day-to-day interaction’, explains Schaart.
Critical look
In this process, it is essential to bring people together who enjoy taking a critical look at the current way of working and to create an environment in which people can feel safe. Schaart: ‘Everyone needs to understand that this is a learning process for everyone and there’s no need to be scared of asking ‘stupid’ questions.’
Within HollandPTC itself, it is possible to test and improve technological innovations on a relatively small scale. ‘New plans often develop from the bottom-up, when a few people come up with an idea together’, says Schaart, ‘and that’s what we’re attempting to facilitate’. Research is also facilitated by a special proton beam that is used solely for research, for example to determine the doses that actually end up in tissues. Researchers also have access to the medical infrastructure in the clinic, including equipment for PET, CT and MRI scans. RST and other TU Delft departments primarily contribute expertise.
Serious long-term effects of gamma radiation
Traditional gamma radiation (with high-energy photons) has also become increasingly targeted over the years, although it is still necessary to irradiate from several sides, which is not the case with proton therapy. This means that gamma radiation is also proving increasingly effective on tumours and patients are living for longer. Despite this, the price they pay for it is greater than was hoped. Because patients live for longer after their cancer treatment, the long-term effects of that treatment are becoming clearer. And these can be very serious indeed. Around 60% of patients aged 30 to 50 with a relatively benign brain tumour are no longer able to do any paid work ten years after all their treatments and around 20% are no longer even capable of living independently.
It is hoped that proton therapy will have fewer serious long-term side effects than gamma radiation. ‘If you irradiate a patient’s abdomen with photons, 40% of the radiation comes out at the back of his body again. In the case of protons, that is 0%. The radiation doesn’t have any further impact even right behind the tumour’, explains Van Vulpen.
Baggage checks
In other words, if you use protons, it is possible to achieve very accurate targeting. ‘That’s great, but you do need to hit exactly the right spot’, says Schaart. ‘The place where the protons’ energy is released can easily be influenced by minor body movements, such as breathing, air bubbles passing through the intestines or the shrinking of the tumour itself’, adds Van Vulpen.
The careful monitoring of a tumour during traditional irradiation is already possible with MRI-guided radiotherapy. However, this requires very complicated and expensive equipment. ‘The challenge we face is to make it easier and cheaper and to achieve that, we aim to improve the quality of the x-ray images currently being used. With a better detector, we hope to be able to make the tumour just as visible as it is with MRI’, explains Schaart.
To do that, he is working on a variation on a technique currently used for baggage checks at Schiphol airport, for example. ‘They irradiate your suitcase using x-rays with different energy levels in order to detect substances like drugs or explosives in a very targeted way. These different energy levels are already produced by the existing x-ray equipment in the clinic. However, the detectors currently in use lack the capability to detect the energy differences. That’s why we’re developing a new detector that can identify all energy levels, which will enable us to create images that show the tumour much more clearly. It’s a bit like advancing from black-and-white to colour photography.’
This idea would never have come about without the collaboration between engineers and medical experts. Schaart: ‘You need to have regular conversations with people from the clinic to find out what the really important questions are.’
*dd 28-03-2023 Marco van Vulpen no longer fulfills the role of director