Preventing hospital-acquired pressure ulcers are a known challenge, requiring a bundle of measures with technical and social elements. Little is known on how the system of prevention policies functions, and which elements and dynamics matter in the eventual outcome. Understanding this is crucial for a hospital both economically and in terms of human suffering. Simon ter Laak, Complex Systems Engineering and Management student dived into the topic in his thesis project.
Pressure ulcers are injuries to skin and underlying tissue resulting from prolonged pressure or pressure in combination with shear. Even though pressure ulcers have received a lot of attention recently in hospitals and long-term care homes, they still form a major issue. Erasmus MC is one of the hospitals with concerns regarding pressure ulcerations. It wanted to find out what is needed to successfully implement measures for improving the prevention of pressure ulcers in the hospital.
Why did you choose to work on this topic?
As part of the search for a thesis, I focused on who I would like to have as supervisors. I approached Dr. Irene Grossmann for thesis topics, because she significantly helped me to improve my academic writing by actually failing me for her class. The feedback I received from her was really helpful and I was intrigued by her direct yet positive style of reviewing my work. She connected me with her contact at Erasmus MC, Dr. Marieke Kruip. It gave me the opportunity to apply the systems thinking methodology from my master Complex Systems Engineering and Management on a relevant case at the hospital: the prevention of pressure ulcers.
As an upcoming engineer, I saw that the fields of healthcare and engineering have so much to learn and gain from each other. The compassion and service towards people and patients in healthcare appeals to me. That made me enthusiastic and eager to get involved in this research.
Why is this research necessary?
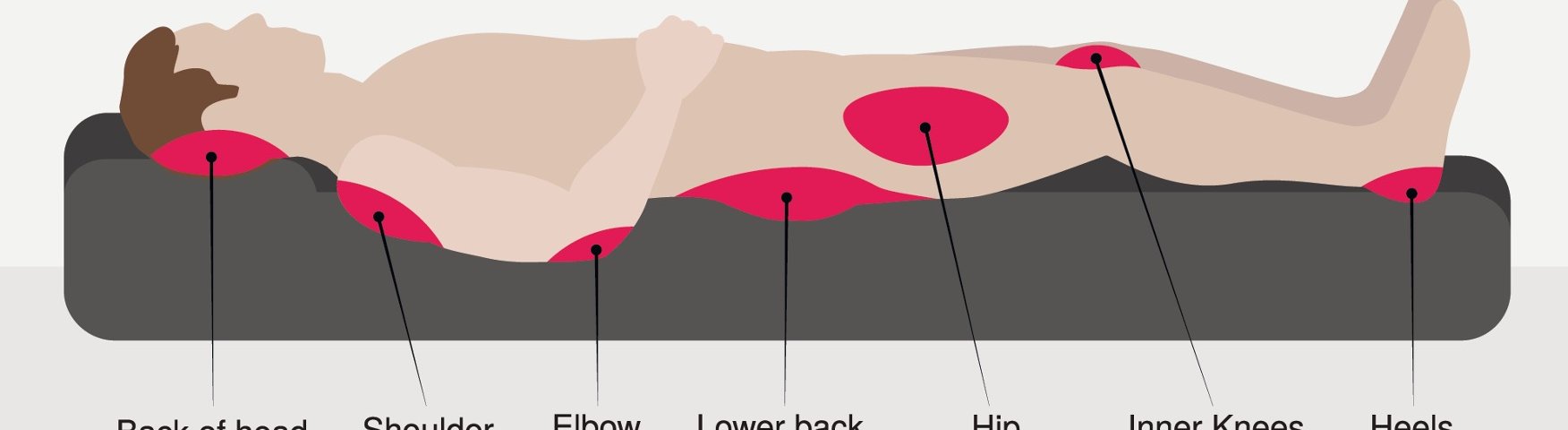
Pressure ulcers are caused by structures (bones, cartilages, tendon) and external stiff support surfaces (e.g., mattresses or seats), or contact with medical and other devices (e.g., common objects “lost” in the bed such as a mobile phone). Pressure ulcers most often occur over bony areas like the sacral and hip regions in adults, with the lower extremities being affected in fewer than 25% of cases.
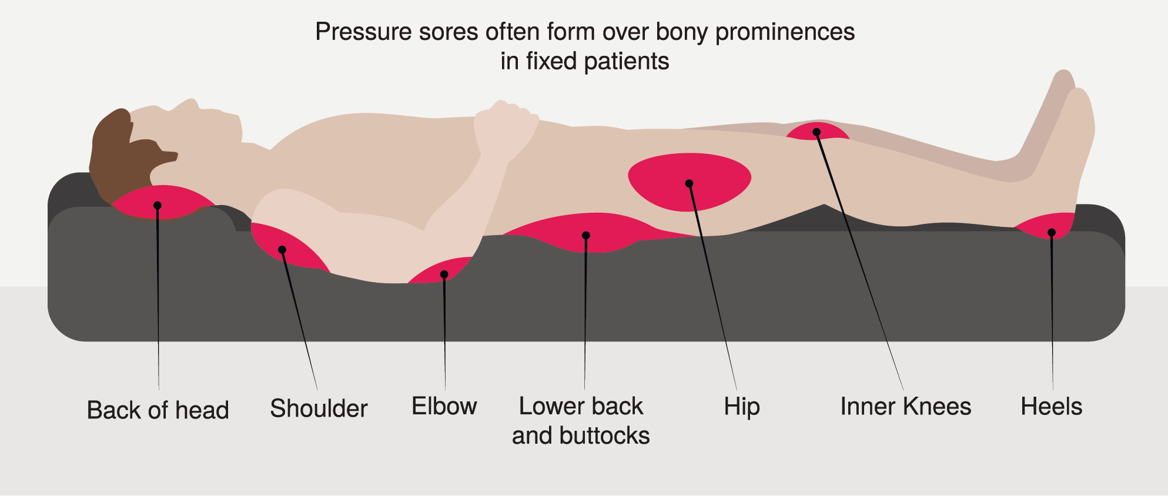
There are numerous support systems, such as pillows, mattresses, and beds, available for the prevention of pressure ulcers. Also, innovations such as changes in materials, care routines and feeding have been applied to prevent pressure ulcers. Despite these innovations, and the existing support systems for the treatment of pressure ulcers, it remains a persistent concern in care institutions. Prevention measures can reduce the incidence of pressure ulcers with at least 50%, saving money and reducing human suffering.
What was your research question and how did you answer it?
My research question was: Why are the current measures for the prevention of pressure ulcers not working as expected and intended in the Erasmus MC hospital? Here, the focus was laid on the current measures for the prevention of pressure ulcers work. I found that the concept of systems thinking, and the application of this concept was lacking.
I was immersed in the hospital organisation for 6 months and collected data through observations, interviews, (policy) documents & records, formal registrations, and evaluations.
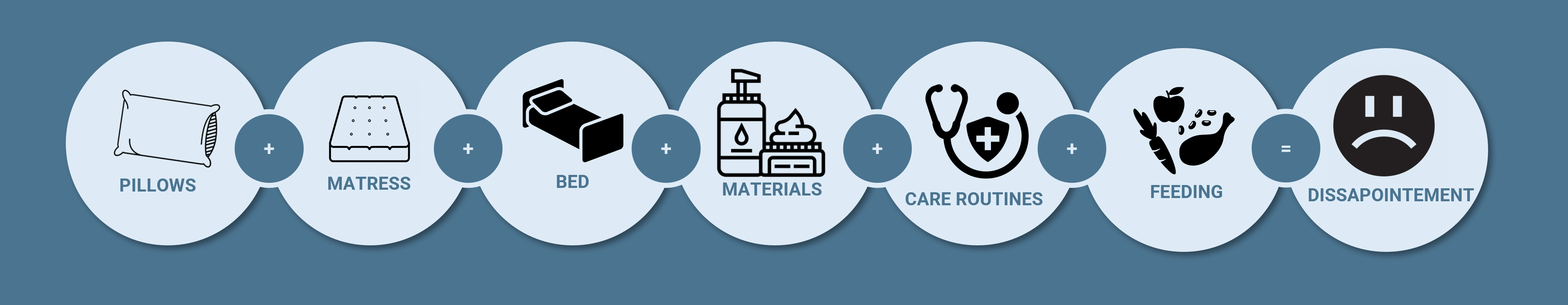
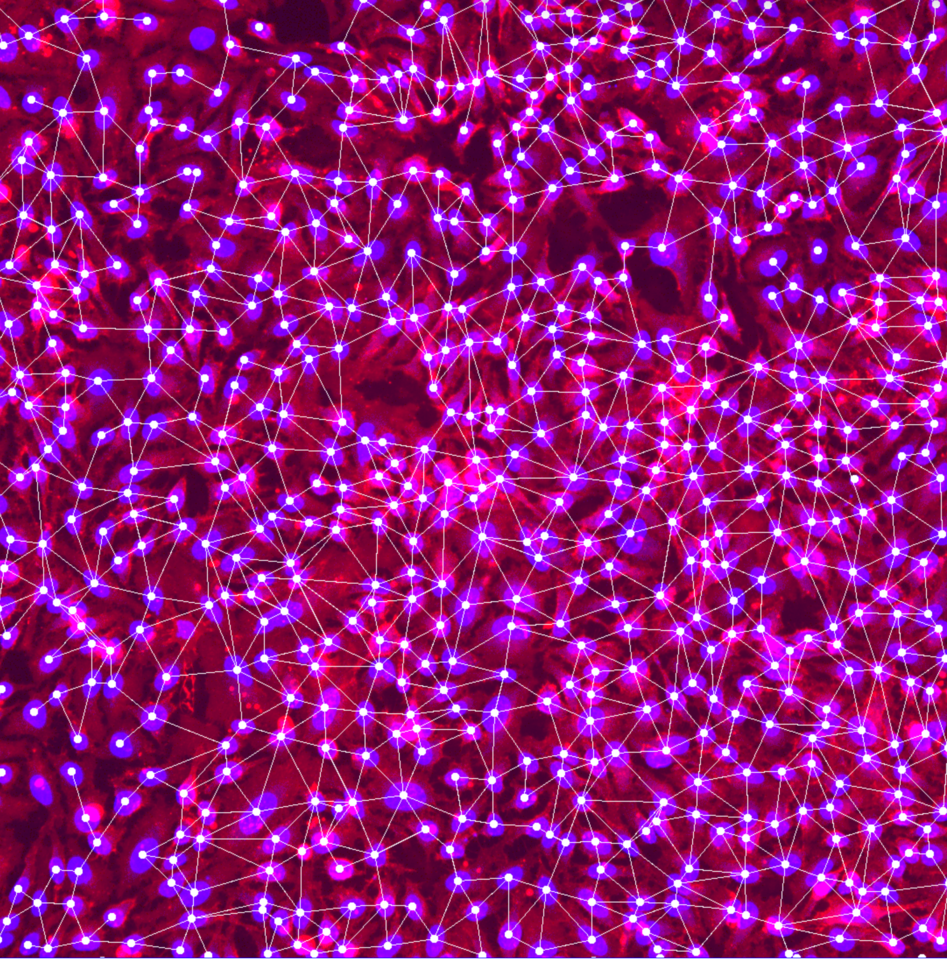
With this data, I created the socio-technical system for preventing pressure ulcers in Erasmus MC. In such a system the social aspects of people and society and technical aspects of organisational structure and processes come together. From the interconnectedness of the system elements, I identified four key leverage points for the system:
- Communication
- Implementation strategy
- Attitude & management style
- Responsibility
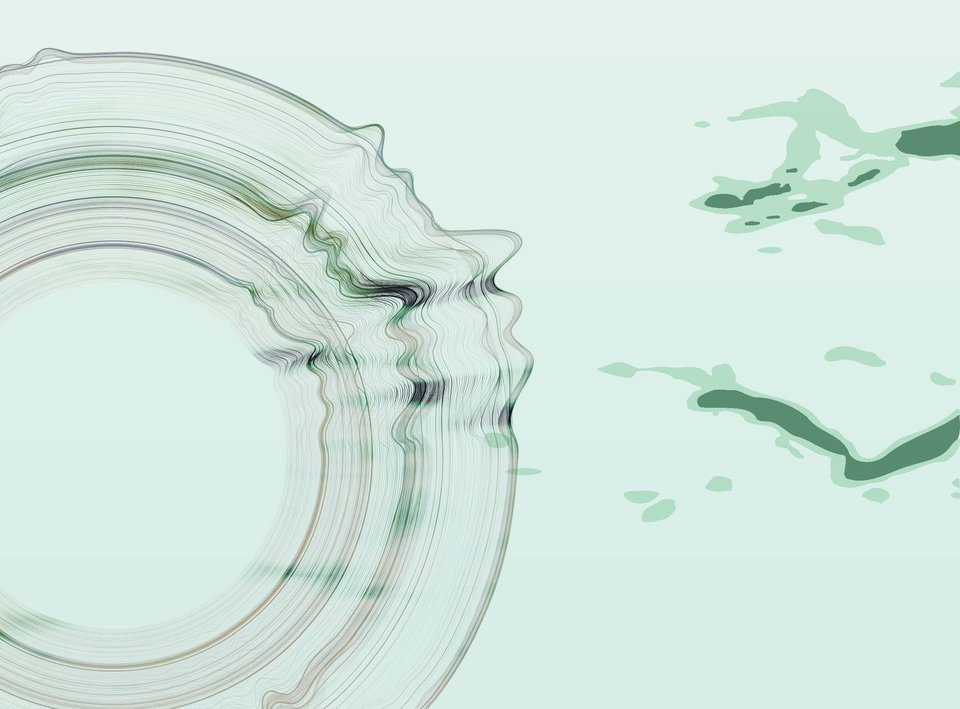
Information-related actor patterns are key in improving the effectiveness of prevention measures. I showed that there is a crucial role for information and the flow of information in an organisation in accelerating and slowing down in diffusion and breakthrough of new technologies.
My experience at Erasmus MC
At the beginning of the case study, I was assigned to the department of Kwaliteit & Patientenzorg in the Erasmus MC. On the first day, I received an Erasmus MC card so I could get around in the hospital. Next to this, I could wear an ErasmucMC nursing outfit to blend in with hospital personnel. I was not allowed to participate in any activities involving patients. This meant that I could not give a helping hand or intervene when care was needed or given to patients. I was only there to observe or ask questions to medical personnel.
I got the opportunity to shadow staff at various departments, which was amazing. I saw nurses, doctors, and policymakers in action inside the hospital. I even got the opportunity (with the right permission) to see a real-life bypass operation. For a case study it is really important to be a “fly on the wall” sometimes to gather solid information. Erasmus MC made it possible for me to gather the information needed for the research.
Erasmus MC is an enormous hospital with more than 15.000 people working there, so getting to know the place was a real challenge the first two weeks. Luckily, the map with routes and building numbers was quite clear and I managed to find everything. Getting on time to appointments and interviews was a bigger challenge and sometimes running was necessary.
What was the main focus in this project?
The main focus of the project was to gather all the information regarding the prevention of pressure ulcers in Erasmus MC, and to find out how to make the current measures for the prevention of pressure ulcers work as expected and intended at the hospital.
From theory, I drafted a first visual representation of the socio-technical system for preventing pressure ulcers in the Erasmus MC. Here, 10 system elements of the socio-technical system were displayed with the current measures for the prevention of pressure ulcers as the artefact(s) of the system. Together with this first visual representation, and the qualitative data I collected in my research, I created the final visual representation of the socio-technical system for preventing pressure ulcers in Erasmus MC. From the key leverage points found within the system, I made several recommendations. Examples of these recommendations are:
- Improve communication by implementing chain consultations between departments and removing one management layer to enhance horizontal and vertical communication.
- Enhance the implementation strategy by hiring an implementation coach, implementing a coherent approach, improving the visibility of quality advisers for nurses, and creating a strategy for implementing the bundle of measures.
- Foster trust in managers and establish a facilitating role among managers to positively influence the attitudes and responsibilities of operational staff and managers.
Did you apply topics from your Master course?
Yes! I used the theory of the multi-level perspective to make the visualisation of the socio-technical system. This was discussed in a course of the Transport & Logistics track in the first year (Innovations in Transport and Logistics) which was actually taught by my other supervisor Jan Anne Annema. Since it was never applied to a healthcare setting, I wanted to try and implement it, and did so successfully!
My courses from the Transport & Logistics track helped to know about the theory of the multi-level perspective by Geels, writing a literature review really helped my English academic writing skills, and finally the course Master Thesis Research Design helped with the start and final version of my thesis.
How does this case study align with your Master course?
The concept of systems thinking is taught throughout the entire Master’s programme. Starting with the bootcamp in the first week, we get to know socio-technical systems and the way actors behave in such a system. I chose the Transport & Logistics track because of my affiliation with the optimization of processes I got from my Bachelor of Industrial Engineering and Management at the Hague University of Applied Sciences. Applying the theory to the healthcare sector was really surprising and it was really cool to see that it could help in a real life setting.
Which topics did you miss from your education?
Knowing how to carry out a case study. This was the first time for me to collect and analyse qualitative data. We learn a lot about the methods to analyse these types of data, but actually gathering the data and doing the research is something different and often overlooked in the education at the university.
What is the most important thing you have learned?
Kill them with kindness. Don’t be afraid to speak up when necessary but always have a smile and try to be positive. Especially in a hospital where you do not have any medical experience and the people are questioning what you are doing there. I have learned that being honest, open, and always being kind to people helps you a long way. It also helps to know the right people that can help you in tough situations. And be prepared! Preparing on how to protect your data and having signed agreements between the hospital and the TU Delft really helps when encountering people who question your methods.
What was the biggest challenge?
The biggest challenge probably was to be able to speak to everybody. Some people are just not approachable or for example do not read their e-mails. This can be a challenge if you really want their perspective. Also, I wanted to speak to as many as people as possible and you just can’t have them all. Interviewing 15.000 people in six weeks is just not going to work… Luckily, I was very fortunate enough to collect a lot of data.
What did you enjoy most?
Being amongst the nursing staff. I was really impressed by the level of professionality and adaptability of nurses in the hospital. Even with policies and instructions all over the place, they were always focused on patients and how to give care that was needed to every individual patient.
The whole experience was great. As someone with no medical degree, experience, or knowledge I was able to participate and see so much in the hospital. I got the opportunity to feel and see what it is like to be a part of an enormous hospital with many hard working people. It was a once in a lifetime experience for me which I will always cherish.
What will happen with the learnings of your case study?
I presented the project to the team of Kwaliteit & Patientenzorg and had an open discussion on how my project could contribute to the policy of preventing pressure ulcers at the hospital. Next to this, I was able to present my findings for a room full of researchers and experts in the medical field during the launch of the TU Delft Institute for Health Systems Science. And as a big bonus, I will publish a paper about my research together with my supervisors Dr. Irene Grossmann and Dr. Jan Anne Annema.
The information I gathered during my case study is full of other interesting leads than just the prevention of pressure ulcers, that will probably be used for future research. Furthermore, I made a contribution to the existing theory of the multi-level perspective, namely the information-related patterns. This could be used in future studies to prove if it is a correct contribution or if it is only applicable to the case study I have performed.